Blog

Labıoplasty
2024-12-17Labioplasty is a surgical procedure to reduce the size of the inner labia. It is recommended for women who are aesthetically uncomfortable with their inner labia, have difficulty wearing tights or bikinis due to their size, experience self-confidence issues, or suffer from recurrent yeast infections.

Vagınoplasty
2024-12-17Vaginoplasty is an aesthetic surgical procedure performed to correct vaginal widening and sagging caused by factors such as childbirth and aging.

Clıtoroplasty
2024-12-15Clitoroplasty is a surgical procedure to remove excess and folded tissues from the area above and around the clitoris.

Genıtal Whıtenıng
2024-12-04The genital area may darken due to factors such as pregnancy, waxing, and recurrent genital infections. There are several methods available for genital whitening.

Genıtal Laser, Prp Applıcatıon, And Orgasm Shot
2024-12-04Genital laser treatments are used for vaginal tightening, genital whitening, removal of warts, and management of recurrent yeast infections. By applying high heat to tissues, the procedure stimulates rejuvenation, tightening, and revitalization of the area.

Barbıe Vagına Surgery
2024-12-04The goal of Barbie vagina surgery is to ensure that no excess tissue is visible when the legs are closed, while standing, or in a seated position. During the procedure, the inner labia are shortened as much as possible, excess folds around and above the clitoris are removed, and fillers are applied to the outer labia if needed.

Uterıne Myomas
2024-11-04Uterine myomas are benign tumors of the uterus. They are observed in 20-25% of women over the age of 35. Myomas often cause symptoms such as bleeding and pain.

Laparoscopıc Hysterectomy
2024-10-04A hysterectomy can be performed using either open or laparoscopic (minimally invasive) methods. The choice depends on factors such as the size of the myoma, previous abdominal surgeries, and the surgeon’s experience. At our hospital, we typically prefer laparoscopic hysterectomy.

Genıtal Fıllers
2024-07-04Genital fillers are used to address wrinkles and volume loss in the outer labia. Wrinkling and sagging in the outer labia can occur due to aging or weight fluctuations. These issues are corrected through filler applications.

Perıneoplasty And Hymenoplasty
2024-07-04Perineoplasty is a procedure to correct scars caused by tears or incisions in the perineal region during childbirth. These scars can be bothersome for women. The unsightly areas are removed and re-stitched to restore the appearance.

Monsplasty
2024-07-04Monsplasty is a surgical procedure to remove excess skin and subcutaneous fat tissue from the mons region. The mons pubis is the triangular area known as the bikini region, located above the outer labia.

Laparoscopıc Myomectomy
2024-01-04Myomas can be removed using either open or laparoscopic (minimally invasive) methods. At our hospital, we perform laparoscopic myomectomy.

Childhood obesity
2023-07-04Childhood obesity, also known as pediatric obesity, is the most prevalent childhood disease worldwide in recent years.
Heart Diseases
2023-07-01Obesity is not just a problem that affects our appearance; it also has serious implications for our health.

Ozone Therapy
2023-06-28Ozone Therapy accelerates your weight loss process by breaking down fat cells in the body and reviving your metabolism.

Gastric Botox is a non-surgical and effective method.
2023-06-25Gastric Botox is a non-surgical and effective method. This injection procedure, easily performed through gastroscopy, takes only a few minutes and usually allows you to be discharged on the same day.

A swallowable gastric balloon is an effective and non-surgical method that provides support in your weight loss journey.
2023-06-20A swallowable gastric balloon is an effective and non-surgical method that provides support in your weight loss journey.

What is Dumping Syndrome?
2022-01-14Dumping syndrome, which is almost never seen after gastric sleeve surgery, is the most important complication seen after gastric bypass surgery.

Why Protein is Important after Bariatric Surgery?
2022-01-13Protein is an important component of every cell in the body.Hair and nails are mostly made of protein. Your body uses protein to build and repair tissues. You also use protein to make enzymes, hormones, and other body chemicals. Protein is an important building block of bones, muscles, cartilage,skin, and blood.
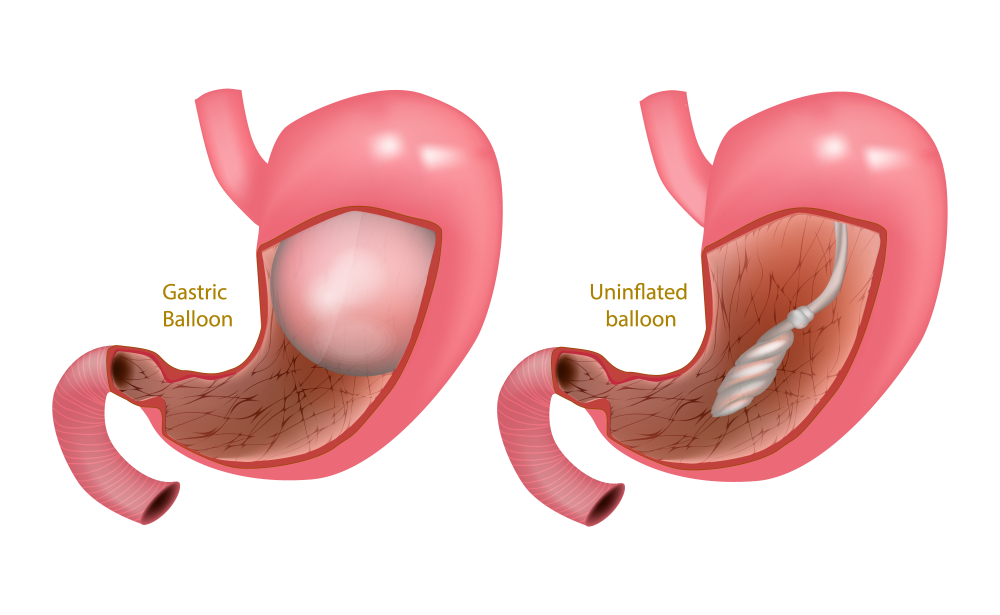
Gastric Balloon
2021-12-17Gastric Balloon is placed into the stomach in a simple, non-surgical outpatient procedure. First, a diagnostic endoscopy is done to ensure that there are no contraindications and that it is safe to perform the procedure. Once you are mildly sedated and comfortable, the procedure can begin.

8 Reasons Why Turkey is the Best Destination for Medical Tourism
2021-12-11For desades, Turkey has always been a well-known tourist destination in the world especially for its historical places,amazing cuisine,wonderful beaches,its art and craft and the most modern resorts. Every year,nearly thirty million tourists visit the country to explore its natural and architectural beatuty. And medical tourism in Turkey has also become one of the most popular choice for patients who seek medical treatment abroad.
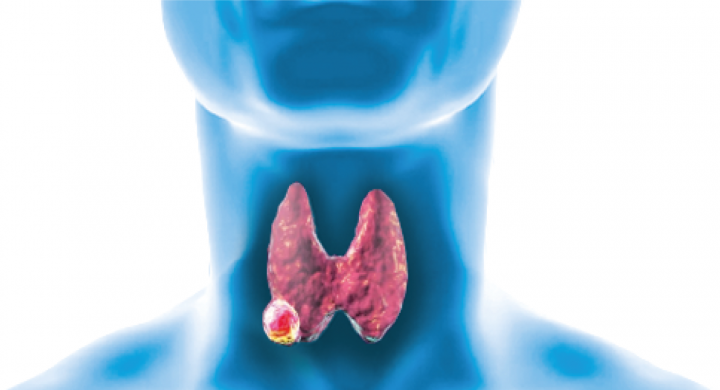
Thyroid Cancer Awareness
2021-11-11Thyroid cancers, differentiated thyroid cancers, medullary thyroid cancer and anaplastic thyroid cancer are divided into three main groups. It is the most common group of differentiated thyroid cancers and accounts for about 95% of all thyroid cancers.
Gastric By-pass
2021-11-03In gastric bypass surgery, a large part of the stomach is bypassed and a small voluminous (approximately 30-50 cc) gastric section is prepared and stitched in the small intestines.In this operation, gastric bypass aimed to reduce the volume of the stomach as well as to disable some of the intestines and throw some of the consumed food unabsorbed as it is in other obesity surgery operations.

How Obesity Affects You and People around You
2021-10-06As frightening and malignant as obesity seems, is a reversible. Obesity can be defined as a condition where patients put on an excessive amount of fat. In such a condition, moving around is difficult, and patients might need help with daily personal activities. This goes to show that not just the patient, but patient?s loved ones too, are easily affected by obesity. issues, etc.

Eating too fast can lead to health problems
2021-09-15Eating too fast can lead to health problems. Nutrition and Diet specialist, Dietitian Lalenur BALCI informed about eating fast habits.?Recent research has shown that, to regulate the body's energy state; body is using neurons.

Stomach Botox
2021-09-08After an average of 15-20 minutes of application, the appetite and the muscles of the stomach, which are effective on hunger, are ineffective for 4-6 months, reducing appetite.

HAIR LOSS AFTER BARIATRIC SURGERY
2021-09-03Hair loss after bariatric surgery is very common and very stressful. In general hair loss is start suddenly and rarely lasts longer than 6 months .

Back Pain, Causes And Surgical Treatment
2021-08-18Nowadays, 85 out of 100 people complain of low back pain. 80 percent of patients with low back pain recover spontaneously within 1 month.Lower back pain is very common.

Packing List For Hospital
2021-07-09The list of suggested things to bring during your recovery in the hospital after surgery can be as large or small according to what you want to carry. We suggest you carry with the essential, especially if you are traveling from afar. The overall patient experience is that they pack a lot more things than what they actually need for a short stay of 3 or 4 nights in the hospital.

Revisional Bariatric Surgery
2021-07-0810% of all obesity operations performed in the world there are possibilities like?fail to get the desired result or have a reverse situation?
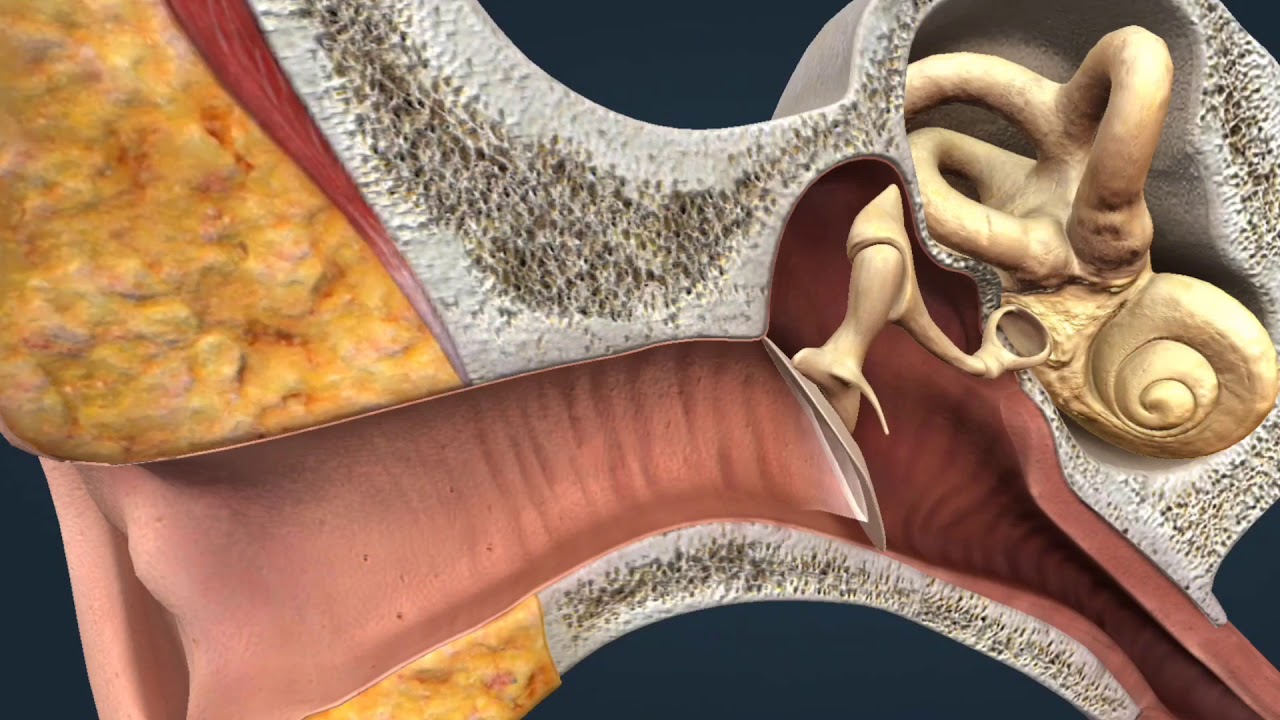
MIDDLE EAR INFECTIONS
2021-06-14The outer ear forms the pinna and ear canal. Deep in the ear canal is the eardrum that separates the outer ear and the middle ear.

Medical tourism is not a complicated process
2021-01-18Medical tourism is not a complicated process. You just need professionals to assist you. We will give you all the support you need before your medical journey.

5 Myths and Facts about Bariatric Surgery
2020-01-27With obesity at epidemic levels, many people consider bariatric surgery. Yet, myths about bariatric surgery keep many people from pursuing this procedure which is an effective way to treat this disease. The long-term success of Bariatric surgery can only be determined if you manage to bring permanent reforms in your lifestyle.
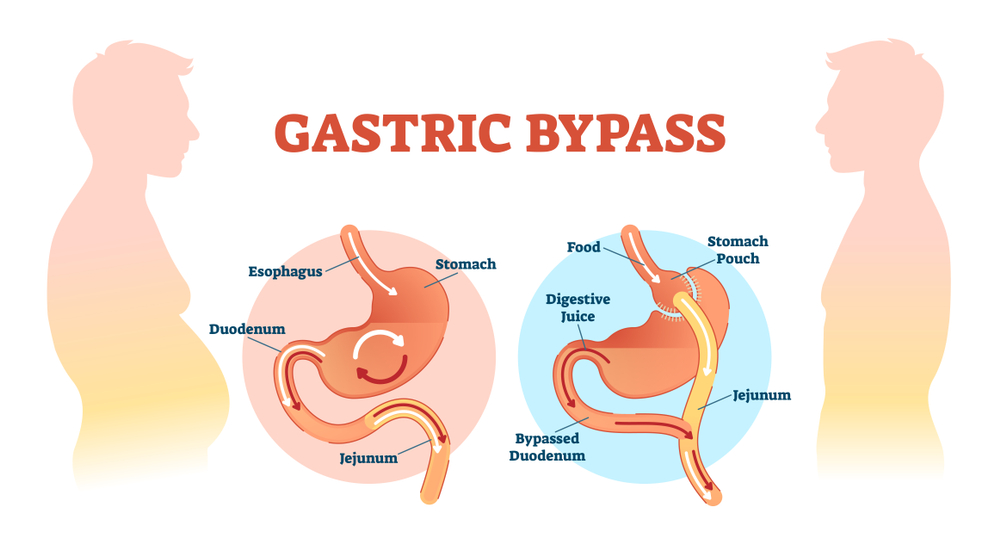
GASTRIC BYPASS
2020-01-12In gastric bypass surgery, a large part of the stomach is bypassed and a small voluminous (approximately 30-50 cc) gastric section is prepared and stitched in the small intestines.In this operation, gastric bypass aimed to reduce the volume of the stomach as well as to disable some of the intestines and throw some of the consumed food unabsorbed as it is in other obesity surgery operations.Thus, patients are fed with less food, and a portion of the food they consume is absorbed.

SLEEVE GASTRECTOMY
2020-01-051. What kind of operation is laparoscopic sleeve gastrectomy surgery? Sleeve gastrectomy is also called ?longitudinal gastrectomy? or ?tube stomach? at the same time.By cutting out the large side of the stomach a volume of 80-85% reduced stomach tube is created. Laparoscopic sleeve gastrectomy surgery, There are 2 mechanisms to lose weight:Mechanical restriction with reduction of gastric volume and weight loss due to reduction of stomach movements, ...
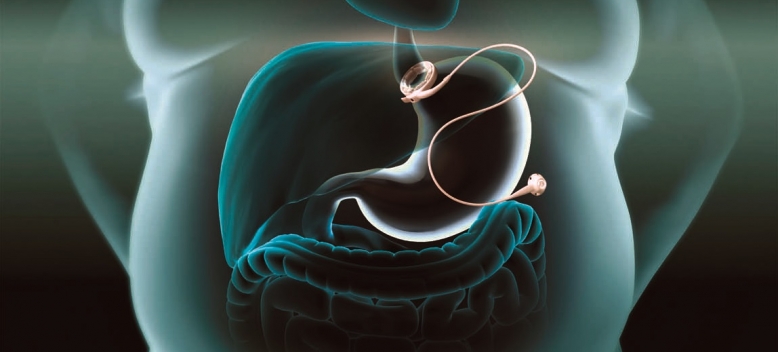
What is Gastric Band Procedure?
2019-01-05The Gatric Banding System, otherwise known as Lap Band or Lapband, is a device that can be placed around the first part of the stomach during ?key-hole? (laparoscopic) surgery for weight loss.